FY26 Health Budget: What Changed and What It Means on the Ground
Brought to you by Bonne Fire ATL
After a year of uncertainty, Congress finalized the FY26 funding package, offering long-awaited clarity for the public health, community health, research, and care delivery systems that underpin how health outcomes are supported across the country.
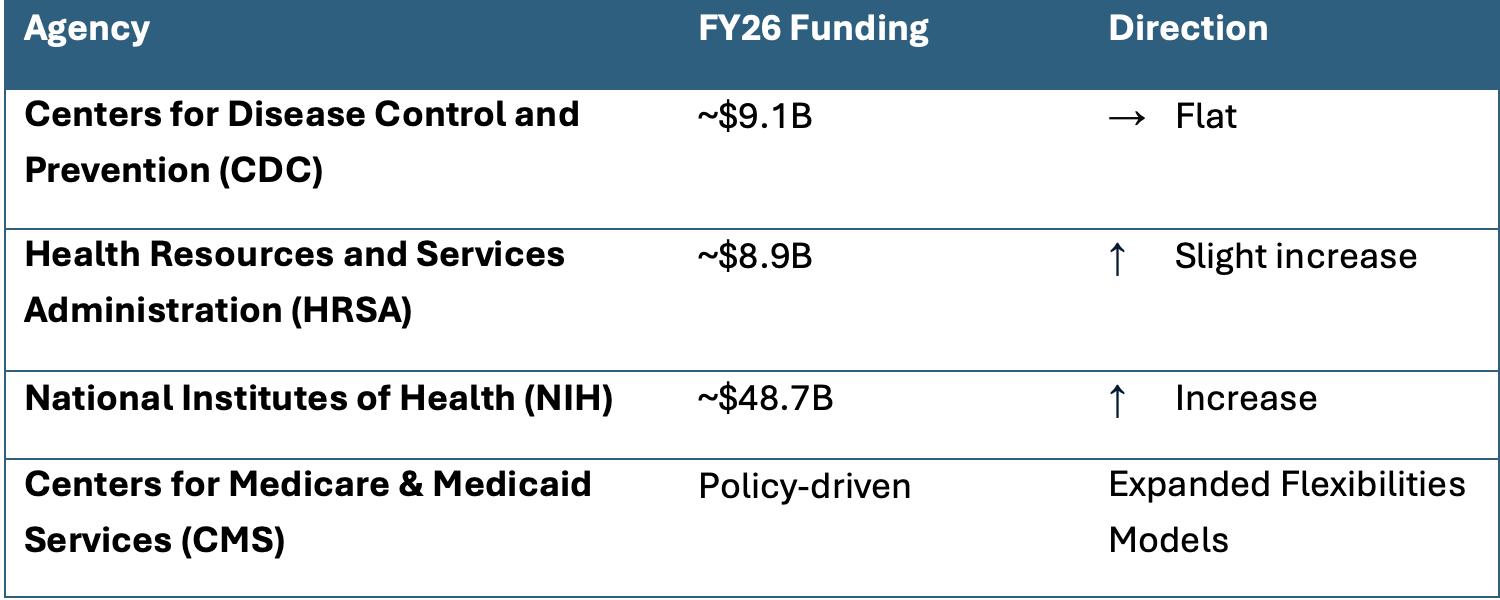
Big Picture: Agency Funding & Direction
*NIH totals are based on Senate and conference summary language indicating a modest increase; final public line-item detail is still emerging.
Why This Matters
The FY26 budget reflects a choice to hold the line rather than significantly expand or reform the system. At a time when some proposals would have sharply reduced federal health capacity, avoiding cuts is meaningful. At the same time, it is a reminder that stability alone does not address long-standing gaps or growing demand.
Community Impact
For communities, this level funding may prevent additional disruption, but does not resolve long standing capacity gaps. Many health departments and providers will still be operating at or near capacity, managing backlogs, workforce shortages, and rising demand with limited new resources.
Opportunities for Innovators
Innovation in this environment is less about launching something new and more about:
Helping existing systems work better with what they have
Reducing friction, duplication, and inefficiency
Supporting continuity rather than transformation
Solutions that assume abundant resources or rapid scale may struggle to land.
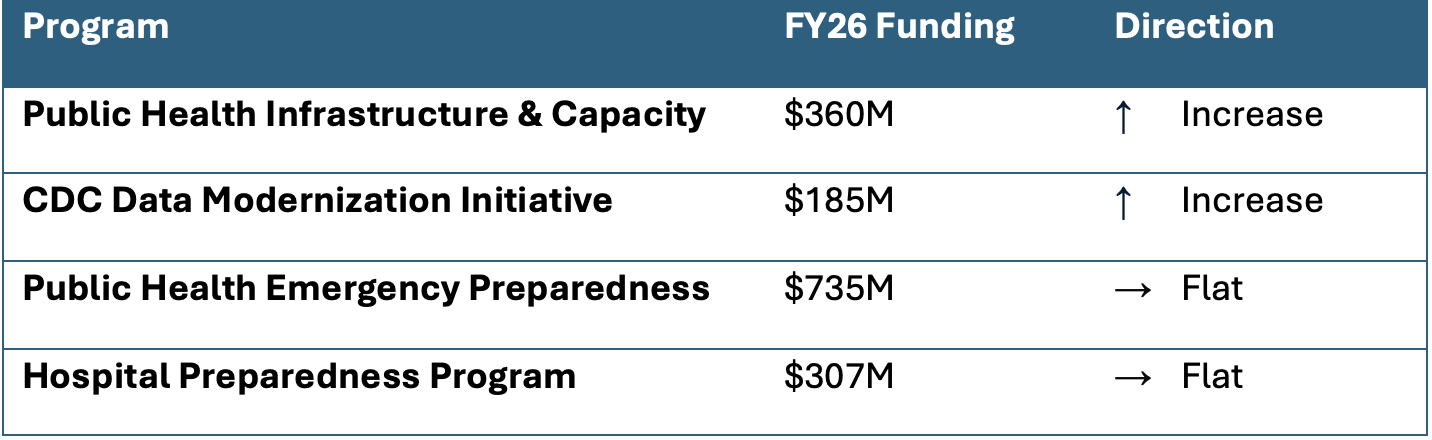
Public Health Infrastructure: Quiet but Consequential
Why This Matters
Investments in infrastructure signal recognition that public health depends on people, data, and readiness. However, the scale of funding points to maintenance rather than rebuilding. These are incremental improvements added to systems that are still stretched thin, especially at the state and local level.
Community Impact
Communities may see modest gains in data timeliness or coordination, but gaps will persist — especially in rural and under-resourced areas. The unevenness of capacity across jurisdictions is unlikely to narrow quickly.
Opportunities for Innovators
There are opportunities for tools that help local agencies use data, not just collect it, regional coordination and situational awareness platforms, and workforce-support solutions that acknowledge staffing constraints.
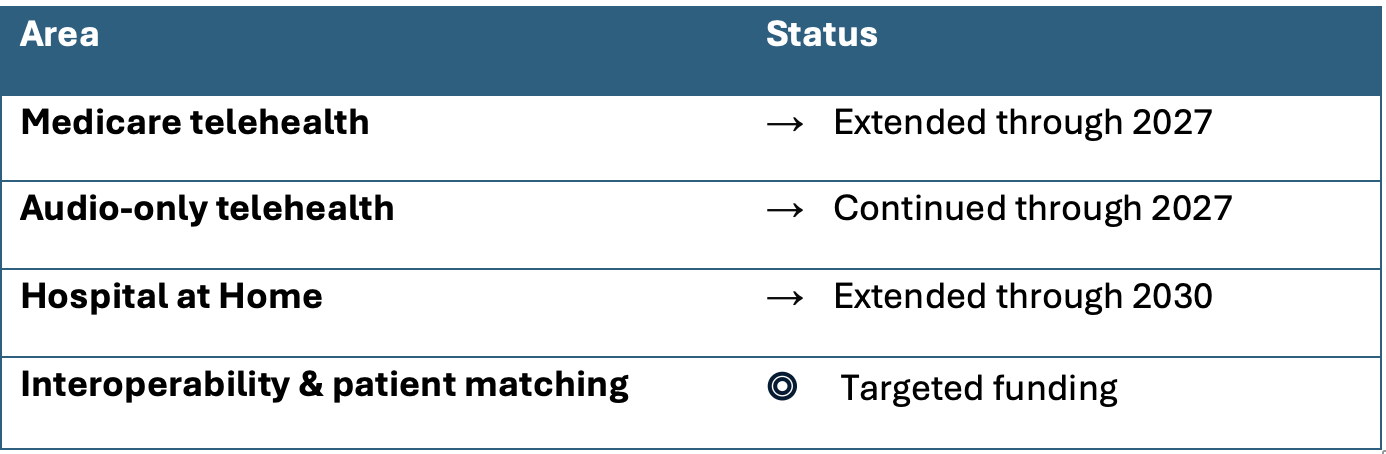
Health Innovation & Care Delivery: From Temporary to Table Stakes
These policy extensions are confirmed through CMS and provider association reporting.
Why This Matters
Extending telehealth and hospital-at-home flexibilities reflects a clear shift. Models that began as short-term or emergency measures are now embedded in how care is delivered. At the same time, extension is not the same as endorsement. Keep going, but prove it works.
Community Impact
Access gains made during the pandemic are preserved, which matters particularly for behavioral health and rural care. But extension alone doesn’t address quality variation, digital divides, or workforce burnout tied to virtual care.
Opportunities for Innovators
The moment seems ripe for:
Solutions that show measurable outcomes, not just utilization
Tools that support clinicians (reducing burnout)
Models that integrate virtual care into existing workflows rather than adding to fragmented systems
Remember, the bar for evidence and implementation is also rising.
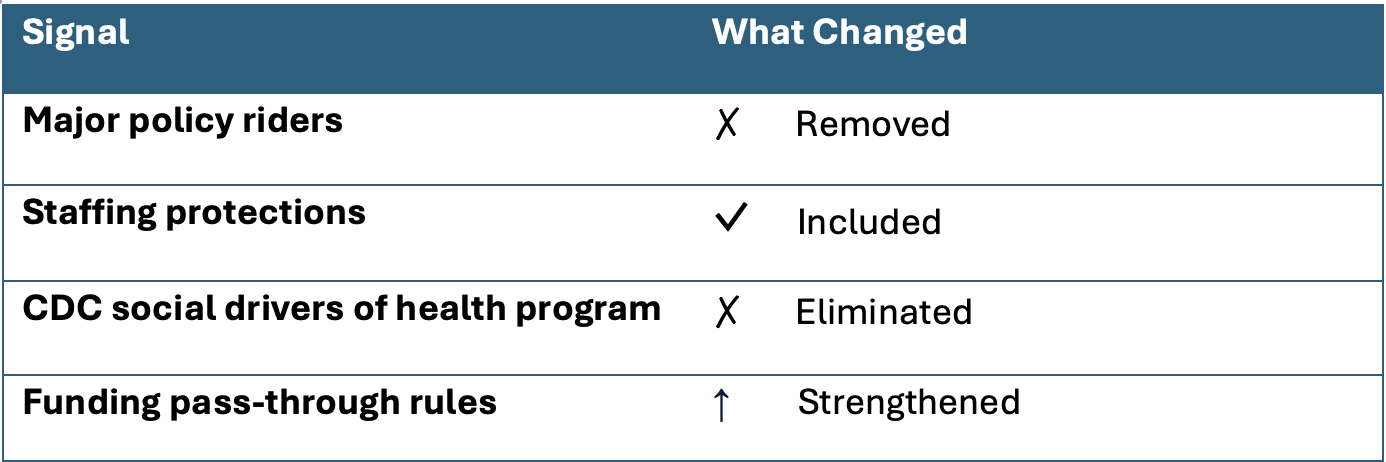
Structural Signals That Shape Implementation
Why This Matters
The removal of major policy riders reduces disruption, but it also reflects clear political limits (Policy riders are provisions that attach restrictions or conditions to funding, often limiting how agencies can operate). While fewer riders allow agencies to focus on delivering programs, the elimination of some upstream initiatives shows there is still no broad agreement on how the federal government should address social and economic factors that shape health.
Community Impact
Agencies may face fewer compliance constraints, but reduced federal support for upstream drivers may be felt most acutely in high-need communities without strong local funding alternatives.
Opportunities for Innovators
There is a need for:
Cross-sector collaboration that doesn’t rely on a single funding stream
Locally adapted models that blend health and social support
Incremental solutions that fit within constrained policy and budget realities
The Bottom Line
The past year brought real uncertainty for public health, with shifting priorities, drastic cuts, and moments when foundational systems felt at risk. Against that backdrop, the FY26 health budget does not solve structural challenges, but seems to provide a measure of steadiness.
For communities, that steadiness matters. It preserves core programs, keeps doors open, and gives local leaders a chance to focus on delivery rather than disruption. For those working across public health, clinical care, and health innovation, hopefully this creates space to regroup, align, and move forward together.
Paired with the CMS Rural Health Transformation Program, there is an opportunity to move beyond stability toward progress. Together, these efforts create room for health innovators and public health leaders to connect funding and local capacity into approaches that are more workable on the ground, especially in rural and underserved communities.
The work ahead still requires creativity, collaboration, and honesty about constraints. But progress is more likely when sectors come together — sharing data, building trust, and solving problems in partnership rather than in isolation. Let’s get to it.
-
U.S. Senate Committee on Appropriations
FY26 Labor–HHS conference summary and report language outlining final funding levels and policy provisions.Association of State and Territorial Health Officials (ASTHO)
FY26 Labor–HHS appropriations analysis, including CDC, preparedness, and public health infrastructure funding.National Association of County and City Health Officials (NACCHO)
Budget briefs and analysis focused on implications for local health departments and community health capacity.
Trust for America’s Health
Context on public health funding gaps, workforce challenges, and infrastructure needs.Centers for Medicare & Medicaid Services (CMS)
Policy updates on telehealth flexibilities, hospital-at-home programs, and the CMS Rural Health Transformation Program.Office of the National Coordinator for Health Information Technology (ONC)
Updates on interoperability, patient matching initiatives, and health data policy.Fierce Healthcare
Reporting on FY26 health funding negotiations, telehealth extensions, and provider impacts.